Aug 16, 2025·8 min
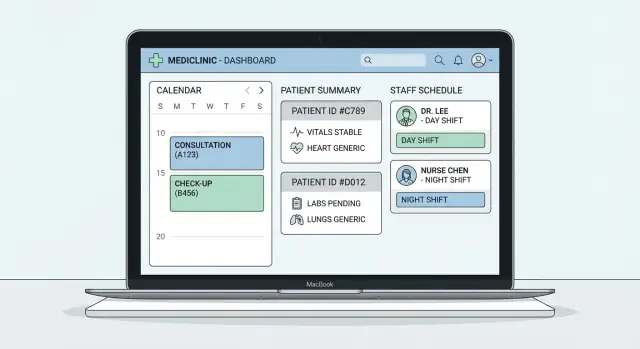
Build a Clinic Web App: Appointments, Records, Scheduling
Plan, design, and build a clinic web app for appointments, patient records, and staff schedules—covering features, data model, security, testing, and launch.
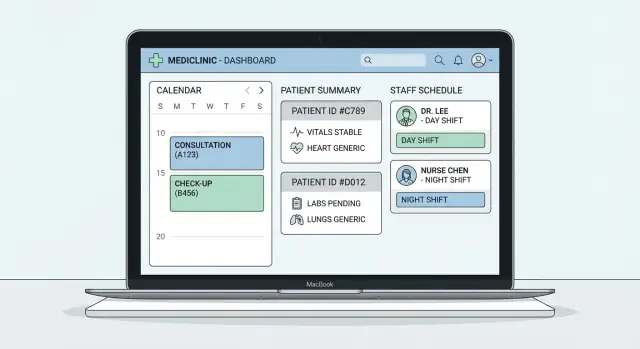
Plan, design, and build a clinic web app for appointments, patient records, and staff schedules—covering features, data model, security, testing, and launch.
Before you write a line of code, get precise about what kind of clinic you’re building for. A solo practice needs speed and simplicity (one schedule, a small team, fewer roles). A multi-location clinic needs location-aware calendars, shared patient charts, and clear handoffs. Specialties add their own wrinkles: dentists may track procedures and imaging, mental health often needs recurring sessions and detailed consent notes, and physio clinics may schedule rooms and equipment.
A practical way to reduce risk here is to validate the scope with a working prototype before you commit to a long build. For example, with Koder.ai you can quickly generate a functional scheduling + records prototype via chat, iterate in “planning mode,” and later export the source code if you decide to take it in-house.
A clinic web app usually has multiple audiences with competing priorities:
Write down the top 2–3 success metrics for each group (e.g., “book in under 60 seconds,” “open chart in under 2 seconds,” “reduce no-shows by 15%”).
List the workflows that happen every day and connect them end-to-end: booking → reminders → check-in → clinical documentation → billing handoff → follow-up. Also include shift planning and coverage changes. These flows quickly surface hidden requirements (time buffers, insurance fields, and who can override schedules).
A focused v1 is easier to launch and safer to validate. Typically, v1 includes appointment scheduling, a basic patient record, and staff availability with simple rules.
Push “later” items—advanced billing, complex clinical templates, multi-location optimization, deep analytics—into a roadmap so they don’t quietly derail your first release.
A clinic web app only feels “simple” when it mirrors how the clinic actually operates. Before screens and features, map the real workflows end to end—especially the messy parts. This prevents building an app that looks polished but forces staff into workarounds.
Start with one complete patient journey and write it as a timeline. A typical flow is:
For each step, note who performs it, what information is collected, and what “success” looks like (e.g., “booking confirmed and reminder scheduled”).
Staff work is more than clicking “Save.” Capture the sequences that create delays and risk:
Even if you won’t build every piece in v1, documenting these flows helps you design screens and permissions that won’t paint you into a corner.
List the exceptions explicitly: walk-ins, no-shows, late arrivals, double-booking rules, urgent visits, provider running late, patients who can’t use email/SMS, and reschedules that happen minutes before an appointment.
Convert each workflow into short user stories (who/what/why) plus acceptance criteria (the conditions to consider it done).
Example: “As a receptionist, I can mark a patient as arrived so the provider sees the queue in real time.” Acceptance criteria might include timestamps, status changes, and exactly who can edit them.
This process keeps your build focused and makes later testing straightforward.
Before you pick a tech stack or sketch screens, decide what your clinic web app must do on day one—and what can wait. Clinics often try to launch “everything,” then struggle with slow workflows and inconsistent data. A clear core feature set keeps medical appointment scheduling, your patient records system, and staff scheduling software aligned.
Start with rules that prevent chaos. Your scheduling should support resources like providers and rooms, time zones for multi-location clinics, and practical constraints such as buffers (e.g., 10 minutes between visits) and visit types with different lengths.
A strong v1 also includes:
Keep the clinical record focused and structured. At minimum: demographics, basic history, allergies, medications, and a place for documents/attachments (referrals, lab PDFs, consent forms). Decide what must be searchable versus stored as files.
Avoid turning v1 into a full EHR replacement unless that’s truly your goal; many apps succeed by handling clinic workflow automation and leaving deep charting to EHR integration.
Staff scheduling should cover shifts, availability, time-off requests, and skill/role requirements (e.g., only certain staff can assist specific procedures). This prevents appointment slots that look “open” but can’t be staffed.
Plan admin tools early: permissions with role-based access control, audit logs for sensitive actions, templates (visit types, intake forms), and configuration for clinic-specific rules. These features quietly determine whether healthcare data security and HIPAA GDPR compliance basics are achievable later.
A clinic web app lives or dies by its data model. If you get the “what is a thing?” and “who owns it?” questions right early, everything else—screens, permissions, reports, integrations—gets simpler.
Most clinic apps can begin with a small set of building blocks:
Resist the urge to add dozens of tables for every form field. Keep a clean “spine” first, then extend.
Write down rules as constraints, not just assumptions. Examples:
This is also where you plan multi-clinic setups: add a Clinic/Organization (tenant) and ensure each record is scoped correctly.
Uploads (IDs, consent forms, lab PDFs, images) should be stored outside your database (object storage), with metadata in the database: type, author, linked patient/encounter, created time, and access restrictions.
Decide retention settings early: what must be kept, for how long, and how deletions are handled.
Use stable internal IDs (UUIDs are common) and keep external identifiers (MRN, payer IDs) as separate fields with validation.
Plan soft deletes (archiving) for clinical data so accidental removal doesn’t break history or audits.
Finally, decide how you’ll handle merges: duplicates will happen. A safe approach is a merge workflow that preserves both records, marks one as “merged,” and redirects references—never silently overwriting clinical history.
Be explicit: the clinic/organization typically owns the record, while patients may have access and rights depending on your policies and local regulations. Ownership decisions drive permissions, exports, and integration behavior later.
Security decisions are hard to “bolt on” later, especially once real patient data is flowing. Start by defining who can do what, then design authentication, logging, and protection of data as first-class features.
Most clinics need a small, clear set of roles: patient, receptionist, clinician, manager, and admin. The goal is least privilege: each role gets only what it needs.
For example, receptionists may create appointments and update contact details, but shouldn’t see full clinical notes. Clinicians should access medical histories for their patients, but not payroll or system configuration. Managers might see operational reports and staffing, while admins handle user management and global settings.
Implement this as role-based access control (RBAC) with a few simple permissions that map to real actions (view record, edit record, export data, manage users). Avoid “everyone is an admin” shortcuts.
Choose an authentication approach early:
Plan session handling: secure cookies, sensible timeouts (shorter for admin functions), and a clear “log out everywhere” option. Staff often share devices at the front desk—design for that reality.
Add audit logs from day one. Track:
Make logs searchable and tamper-resistant, and decide retention rules that match your policy.
Encrypt data in transit (HTTPS/TLS) and at rest (database/storage encryption). Set up automated backups, test restoring them, and define who can trigger restores.
A secure app that can’t recover from mistakes, ransomware, or accidental deletion isn’t secure in practice.
Compliance isn’t a “later” task. The decisions you make about data fields, user roles, logs, and exports will either support privacy requirements—or force expensive rework.
Start with a simple matrix: where your clinic operates, where patients are located, and what your app does (scheduling only vs. storing clinical notes).
Common examples:
Write down what this means in practice: breach notification timelines, access logging expectations, patient rights, and required contracts (e.g., HIPAA BAAs with vendors).
Create a “data inventory” table for each screen and API:
Aim for data minimization: if a field doesn’t directly support care, operations, or legal requirements, don’t collect it.
Prioritize features that reduce risk during daily work:
Use your checklist to drive structured reviews with counsel/compliance:
Treat this as an ongoing process: regulations, vendors, and clinic workflows evolve.
Appointment scheduling is where clinic apps either earn trust quickly—or create daily friction. The goal is simple: staff should be able to see availability at a glance, book in seconds, and feel confident nothing will collide behind the scenes.
Start with day and week views, because that’s how most front desks think. Make time blocks large enough to read, and keep the “create appointment” action one click away.
Add filters that match real operations: provider, location, and appointment type. If your clinic uses rooms, equipment, or chairs, include a room/resource view so staff can spot constraints early (e.g., “Room 2 is already used for procedures at 11:00”).
Color-coding by appointment type can help, but keep it consistent and accessible.
Common rules to support from the start:
Store these rules centrally so they apply whether the booking is made by staff or later through a patient portal.
Reduce no-shows by sending reminders via email/SMS at sensible intervals (for example, 48 hours and 2 hours before). Keep messages short and include clear actions:
Make sure every action updates the schedule immediately and leaves an audit trail staff can reference.
Two staff members can click the same slot at the same time. Your app must handle that safely.
Use database transactions and a constraint-based approach (for example, “a provider cannot have overlapping appointments”). When saving a booking, the system should either commit successfully or fail cleanly with a friendly message like “That time was just taken—please choose another slot.” This is more reliable than hoping the UI stays in sync.
Patient records are the screen your team will live in all day. If it’s slow, cluttered, or risky to edit, staff will work around it—and that’s where errors happen.
Aim for a chart that loads quickly, is easy to scan, and makes the “right” workflow the easiest one.
Start with a quick patient search that tolerates real-world input: partial names, phone numbers, DOB, and common misspellings.
Once a chart opens, keep the most-used items within one click. Include a “recent visits” panel, prominent alerts (allergies, critical conditions, care plans), and clear access to documents.
Small touches matter: a sticky patient header (name, age, identifiers) and consistent tabs so staff don’t hunt.
Structured forms help when you need consistency: vitals, symptoms, screening questions, medication lists, and problem lists. Keep them short and tailored—too many required fields slows everyone down.
Always provide free-text notes alongside structured fields. Clinicians need room for nuance, context, and exceptions.
Use templates sparingly and let teams customize them by role (front desk vs. nurse vs. clinician).
Support uploading referrals, lab PDFs, images, and consent forms with clear limits (file types and size). Store uploads securely and consider virus scanning if your risk profile or regulations require it.
Show upload status, and avoid “silent failures” that lead to missing documents.
Medical records need a strong audit trail: who changed what, when, and why. Track author and timestamps, store prior versions, and require a reason for edits to signed notes or key fields.
Provide an easy “view history” so supervisors can resolve disputes quickly without digging through logs.
Staff scheduling is where clinic operations either feel effortless or constantly “patched” with phone calls and sticky notes. The goal is to model how your clinic actually works—then let the app prevent problems before they reach patients.
Start with a simple baseline: standard working hours per person (e.g., Mon–Fri 9–5). Then layer real-life exceptions:
Store these as separate rules so you don’t “edit history” every time someone takes a day off.
Most clinics repeat the same rhythm weekly. Add shift templates (e.g., “Front Desk AM”, “Nurse Triage”, “Dr. Smith Procedure Block”) and allow recurring schedules (“every Monday for 12 weeks”). This reduces manual entry and makes schedules consistent.
Don’t rely on staff to notice collisions. Your app should warn or block:
Make conflicts readable (“Conflicts with 10:00–14:00 shift”) and offer quick fixes (“swap”, “assign alternate”, “shorten shift”).
Provide clear views: weekly grid, day timeline, and “my next shifts” for mobile.
Add notifications for changes and lightweight exports (PDF/CSV) so managers can share schedules when needed.
Integrations are where clinic apps either feel “connected” or constantly cause double-entry. Before you write code, make a clear list of systems you must connect to and what data should move between them.
Most clinics end up needing at least a few of these:
When possible, use healthcare standards such as HL7 v2 (common for labs) and FHIR (common for modern EHR APIs). Even with standards, every vendor interprets fields a bit differently.
Create a simple mapping doc that answers:
Prefer webhooks (push updates) over constant polling when available. Assume failures will happen and design for them:
Define a fallback plan: a manual workflow in the UI, an “integration down” banner, and alerts to staff/admins.
Make failures visible, traceable, and recoverable—so patient care doesn’t stall when a vendor API does.
Your architecture should make everyday clinic work reliable: fast pages at the front desk, safe access to patient data, and predictable integrations. The “best” stack is usually the one your team can build and maintain without heroics.
Common, proven choices:
If you expect multiple locations or future modules, consider a modular backend with clear boundaries per domain (appointments, records, staff).
If you want to move fast without locking yourself into a black box, Koder.ai is a practical middle ground: it can generate a React-based web app with a Go backend and PostgreSQL, supports deployment and hosting, and offers snapshots/rollback so you can iterate safely as you validate workflows.
Plan for dev / staging / prod from day one. Staging should mirror production settings so you can test real workflows without risking patient data.
Keep configuration (API keys, database URLs, feature flags) outside the codebase via environment variables or a secrets manager. This reduces “it worked on my machine” issues and supports safer deployments.
Decide whether you’ll use REST (simpler, widely understood) or GraphQL (flexible queries, but more governance). Either way, document endpoints and payloads, validate input, and return clear error messages that help staff recover (e.g., “Time slot no longer available—pick another”).
Clinic apps often slow down as patient records grow. Bake in:
If you’re planning integrations, keep them behind a dedicated service layer so swapping vendors later doesn’t rewrite your core app.
For related planning, see /blog/security-access-control-clinic-app.
A clinic app fails in predictable ways: double-booked appointments, the wrong person seeing the wrong chart, or a schedule change that silently breaks the day.
Treat testing and operations as product features—not chores you “do at the end.”
Start with a small set of “golden paths” and test them repeatedly:
Mix unit tests (business rules), integration tests (API + database + permissions), and end-to-end tests (browser flows).
Keep a realistic set of test users (front desk, clinician, billing, admin) to validate role boundaries.
Automate the basics:
Use CI/CD with a repeatable release process. Practice database migrations in staging, and always ship with a rollback plan (or roll-forward scripts when rollback isn’t safe).
Add monitoring for uptime, error rates, queue backlogs (if any), and slow queries. Define incident response basics: who is on call, how to communicate with clinics, and how to capture a post-incident review.
If you use a platform approach (including tools like Koder.ai), prioritize features that reduce operational risk: one-click deploys, environment separation, and reliable rollback via snapshots.
Run a pilot clinic first. Provide short training materials (5–10 minute tasks) and a checklist for go-live day.
Set up a feedback loop (weekly review, tagged issues, top pain points) and turn it into a clear v2 roadmap with measurable goals (e.g., fewer no-shows, faster check-in, fewer scheduling conflicts).
Start by defining your clinic type (solo vs. multi-location) and specialty needs, then list each user group and their top 2–3 success metrics.
Examples:
Map the full flow end-to-end: booking → reminders → check-in → documentation → billing handoff → follow-up.
Then add the “messy” real-life exceptions (walk-ins, late arrivals, double-book rules, last-minute reschedules) so your app doesn’t force workarounds.
A strong v1 is usually:
Push advanced billing, deep analytics, and complex templating to the roadmap.
Start with a small “spine” of core entities:
Keep relationships and constraints explicit (e.g., no overlapping provider appointments). Extend later instead of creating dozens of tables upfront.
Treat uploads as separate from your database:
Decide retention and deletion behavior early, and use soft deletes/archiving for clinical data.
Define a small set of roles (patient, receptionist, clinician, manager, admin) and implement least-privilege RBAC.
Also plan:
Build a simple checklist driven by where you operate and what data you store.
At minimum, create a data inventory per screen/API:
Use this to support HIPAA/GDPR needs like auditability, “minimum necessary” access, and patient request workflows.
Put booking rules into the system, not staff memory:
Prevent collisions with database constraints/transactions, and design reminders with clear actions (confirm/reschedule/cancel) that update the schedule immediately with an audit trail.
Make charts fast to open and easy to scan:
Make edits traceable with versioning, author/timestamps, and “reason for change” on sensitive edits (like signed notes).
Start with required integrations and define a “source of truth” per data type (your app vs. EHR).
Implementation basics: